Corneal Transplantation for Corneal and External Eye Diseases

An improperly curved cornea may be corrected surgically or non-invasively to reduce or eliminate the need for eyeglasses or contact lenses. A thorough eye examination and consultation are necessary before a treatment decision can be made.
Corneal transplantation, or keratoplasty, is recommended when the cornea’s curvature is too steep or flat to be treated with other methods, or when extensive damage has occurred due to disease, infection or injury.
Common problems that require transplantation are:
- Dry Eyes
- Blepharitis
- Recurrent Erosion
- Corneal Ulceration
- Herpes Simplex Keratopathy
- Pseudophakic Corneal Decompensation
- Keratoconus
- Corneal Dystrophies
- Pterygia
- External tumors
- Eye infections
- Traumatic injury
- Ocular surface diseases
- Chemical burn
Good candidates for a corneal transplant In Honolulu, HI
Corneal eye disease affects over 10 million people worldwide; it is the fourth most common cause of blindness. When disease or injury damages the cornea, it can become swollen, scarred, or severely misshapen, and this distorts the quality of the person’s vision.
In these cases, eyeglasses or contact lenses are used as the first treatment options. But when these can no longer provide the degree of correction needed, a corneal transplant could become necessary. In other cases, swelling can become so painful that a transplant is the only route forward.
These conditions could all be reasons for a corneal transplant:
- An outwardly bulging cornea
- Fuch’s dystrophy
- A thinning cornea
- Clouding of the cornea
- Cornea scarring from injury or infection
- Swelling of the cornea
- Corneal ulcers
- Complications from previous eye surgery
How is Corneal Transplantation Surgery Performed?
Transplantation involves replacing the damaged cornea with a healthy one from a donor (usually through an eye bank). Keratoplasty is a low-risk procedure – it is the most common type of transplant surgery and has the highest success rate.
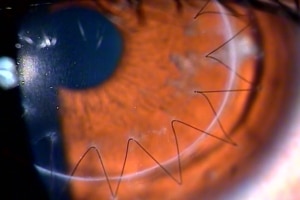
During the procedure, a circular incision is made in the cornea. A disc of tissue is removed and replaced with healthy tissue; these discs may be thin (lamellar keratoplasty) or as deep as the entire cornea (penetrating keratoplasty, the technique used in almost all corneal transplants). Local or general anesthesia may be used. The entire procedure lasts only 30-90 minutes.
The results that can be achieved with a Keratoplasty
A cornea transplant can restore vision, reduce pain, and improve the appearance of a damaged or diseased cornea. What you can expect to achieve with these surgeries with Dr. Maehara depends in part upon the reason you needed the surgery, as well as your overall health.
As mentioned above, your initial vision will be worse than before your surgery. It will take several months for your vision to improve.
Once the outer layer of your cornea has healed, Dr. Maehara will work to make adjustments to further improve your vision, if possible. These may include correcting any unevenness in the cornea (astigmatism). These can be due to stitches that hold your donor cornea in place. Dr. Maehara can release some of these stitches and tighten others. Refractive errors that remain can be corrected with glasses, contact lenses, or, in some cases, laser eye surgery.
Corneal Transplants Performed by Dr. Maehara
Traditional Corneal Transplant (with sutures)
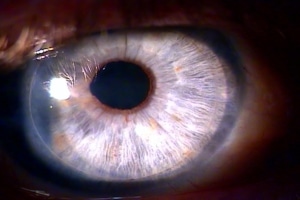
Sutureless Partial Thickness DSEK Transplant.
What is recovery like after a corneal transplant?
Although Dr. Maehara performs mostly penetrating keratoplasty, or full-thickness transplants, he also sometimes performs transplants where he doesn’t replace the entire cornea, but different degrees of its depth.
Because of that there is a different recovery timeframe between full thickness transplants or partial thickness (such as DSEK), but patients need to be patient in either case. Recovery after a cornea transplant takes time, up to a year or even longer. With DSEK, thanks to the lesser amount of transplanted tissue, patients can have their best vision in about three months after their procedure. This can vary by the patient.
In the beginning, your vision will likely be even worse than it was prior to your surgery because your eye takes time to get used to the new cornea. This can be disconcerting to patients, but this is where you need patience. Your vision will improve, and you’ll begin returning to your normal routines.
You’ll use steroid eye drops for several months after your transplant to help your body accept the new corneal graft. You’ll also need to protect your eye at all times with either a shield or eyeglasses; you can’t inadvertently bump your eye.
When you can return to normal activities following a Keratoplasty
Most patients can return to work within a week after surgery, depending on your job and how quickly your vision begins to improve.
You’ll need to be careful with lifting, as you need to avoid increasing blood pressure to the head and face. Heavy, strenuous exercise and lifting are prohibited for a number of weeks; Dr. Maehara will discuss this with you.
Going to the beach will definitely be out for a period of months, maybe longer. You cannot risk bacteria or even sand getting into your eyes. Pools can be even more problematic, due to the bacteria present. The pressure placed on your eyes when you submerge your head is also an issue.
What are the risks involved with corneal transplants?
These are generally safe and successful surgeries, but there are some risks involved. The main risk is that your body rejects the donor cornea. Overall, here are the risks involved with these procedures:
- Eye infection
- Increased risk of developing a cataract
- Pressure increase inside the eyeball (glaucoma)
- Problems with the stitches used to secure the donor cornea
- Swelling of the cornea
- Rejection of the donor cornea
Rejection occurs in about 10 percent of these surgeries. These are possible signs of possible rejection: loss of vision, pain, redness, sensitivity to light.
Schedule Your Consultation Today!
Dr. Jeffrey Maehara also performs a modern version of corneal transplantation called DSEK (descemet stripping endothelial keratoplasty). This is a partial thickness transplant to treat conditions where the inner layer of corneal cells are not healthy and don’t function properly. Only the inner layer of the cornea is replaced through a small incision. This less invasive procedure has the advantage of quicker visual recovery, less induced astigmatism, and less change in the glasses prescription.